Invoicing Overview
Streamline your billing process with intelligent automation and clear reporting. Manage coverage, verify eligibility, monitor credit limits, and generate accurate statements — all within your No Rejects platform.
Overview
Automate and simplify end-to-end billing with integrated claim management and payment tracking.
- Pharmacy assigns Cardholder IDs (typically automatic in PIS)
- Adjudicate claims and COB:
- Calculate pricing
- Check balances and apply coverage rules
- Create invoices
- Trigger autopay
- Schedule or trigger statements and notices
- Receive and apply payments
- Export AR and GL data to accounting systems
Coverage Verification
Ensure coverage validation is accurate before invoicing to reduce denials and rework.
- Most bad debt is due to expectation of insurance coverage
- If a suitable reject is not provided, we reject
- Medicaid Waiver, Hospice, and Group Homes
Example Reject:
NR1> Covered by Part D or Part D reject needed. Other coverage: 123456 PARTD
Credit Limits
Maintain control and accountability by managing credit exposure and automating bad-debt prevention.
- Most bad debt is because of expectation of insurance coverage
- If a suitable reject is not provided, we reject
- Medicaid Waiver, Hospice, and Group Homes
Example Reject:
NR1> Patient past due. Balance $235.05. Last payment 1/22/2025. NR1> Autopay denied: Insufficient Funds
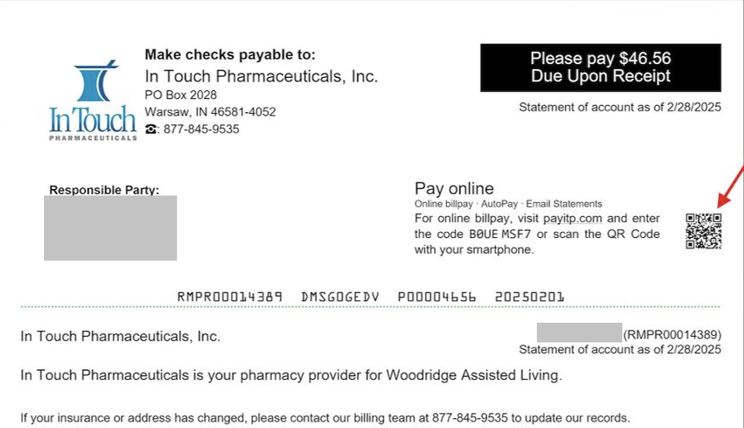
Example Statement
Deliver professional, branded statements for clarity and compliance across facilities.
- Branded for pharmacy
- Facility co-branding available
- Customizable design and contact details